Vital new insights into deadly African sleeping sickness disease
Published: 8 November 2021
A newly published extensive body of research into Human African trypanosomiasis (HAT), also known as sleeping sickness, has revealed new insights into the deadly parasitic disease that threatens the lives of millions of people in 36 sub-Saharan African countries
A newly published extensive body of research into Human African trypanosomiasis (HAT), also known as sleeping sickness, has revealed new insights into the deadly parasitic disease that threatens the lives of millions of people in 36 sub-Saharan African countries.
Led by Professor Peter Kennedy CBE in the University of Glasgow and published in PLOS Neglected Tropical Diseases, the research project has found evidence that questions our current understanding of sleeping sickness as a two stage disease – early and late – with direct impact on how we should both diagnose and treat patients with the fatal disease.
By using a mouse model of sleeping sickness to better understand how the disease develops, the researchers have been able to show that a range of host genes controlling the development of central nervous system disease are activated much earlier than previously thought, and earlier than the development of neurological features of the disease. These crucial findings could explain why neurological features may occur relatively early in the disease – something that goes against the classical two stage disease understanding – and may also explain why parasites can enter the central nervous system so early after initial infection.
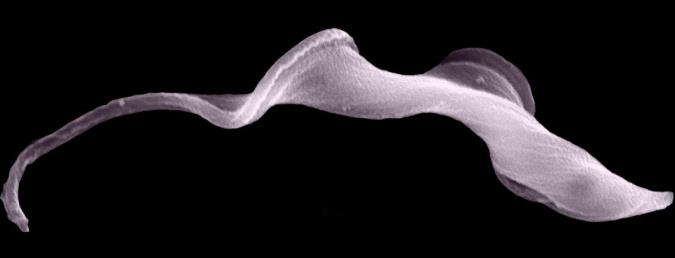
Sleeping sickness, is a major killer disease of sub-Saharan Africa which puts around 70 million people at risk in sub-Saharan African countries. Transmitted by tsetse flies when they bite humans to consume a blood meal, and caused by unicellular protozoan parasites called trypanosomes, sleeping sickness is invariably fatal if untreated or inadequately treated.
Currently, sleeping sickness is understood to have two stages: the early, stage 1, or haemo-lymphatic stage, which is when treatment is effective and relatively non-toxic; the subsequent late, stage 2, or encephalitic stage, when, sadly, current treatments are toxic and can be complex to administer.
According to the WHO criteria the stages of sleeping sickness are based on the presence of a defined amount of white blood cells in the cerebrospinal fluid. However, different groups of physicians in Africa use different staging criteria and there remains no clear consensus as to what constitutes stage 2 disease. Recent studies have reported the occurrence of neurological, or late-stage features in African patients who appear to have no or few cells in the cerebrospinal fluid, which would otherwise categorise their condition as early-stage disease.
Professor Peter Kennedy, senior and corresponding author of the study from the University of Glasgow’s Institute of Neuroscience and Psychology, said: “Our work offers important new insights into this fatal disease, and has potential implications for not only our understanding the nature of sleeping sickness, but our treatment of patients when diagnosed with it as well.
“Finding that host genes controlling the development of central nervous system disease are activated much earlier than previously after initial infection, calls into question the basis of dividing the disease into distinct early and late stages, and indicate that the disease development is complex and depends on a wide range of interacting factors.”
The study, ‘Microarray profiling predicts early neurological and immune phenotypic traits in advance of CNS disease during disease progression in Trypanosoma. b. brucei infected CD1 mouse brains’ is published in PLOS Neglected Tropical Diseases. The study was funded by Wellcome.
Enquiries: ali.howard@glasgow.ac.uk or elizabeth.mcmeekin@glasgow.ac.uk / 0141 330 6557 or 0141 330 4831
First published: 8 November 2021
<< November
Related Links
- Professor Peter Kennedy CBE, profile
- Institute of Neuroscience and Psychology
- College of Medical, Veterinary and Life Sciences
- Wellcome
- Microarray profiling predicts early neurological and immune phenotypic traits in advance of CNS disease during disease progression in Trypanosoma. b. brucei infected CD1 mouse brains, published in PLOS Neglected Tropical Diseases

