New hope for rheumatoid arthritis sufferers
Published: 1 July 2020
A study led by the Institute in collaboration with Fondazione A.Gemelli IRCCS in Italy and RACE has, in the joints of individuals on long-term remission, found the key to swift treatments to cure the pain caused by the condition.
A study led by the Institute in collaboration with Fondazione A.Gemelli IRCCS in Italy and Research into Inflammatory Arthritis Centre (RACE) has found the key to swift treatments to cure the pain caused by the condition.
The research, published in Nature Medicine, found that those with arthritis in long-term remission had a difference in cell function which could settle inflammation and ‘teach’ nearby cells to repair the joint.
Although treatment for rheumatoid arthritis has improved, some sufferers do not respond well, with many having unpredictable ‘flare-ups’ of the disease.
However, scientists now hope that by harnessing the benefit of these ‘resolving’ cells it could lead to new and more effective treatments.
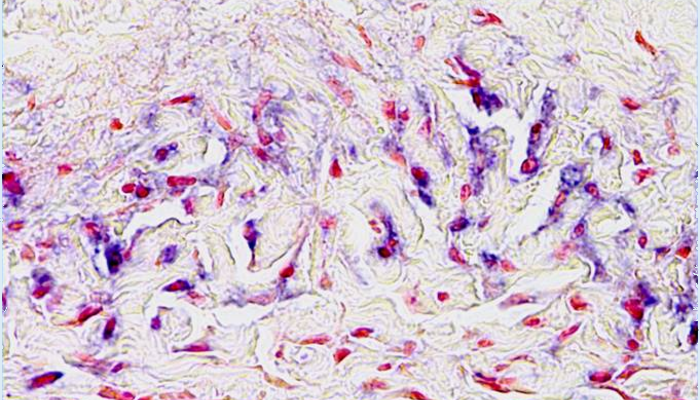
The study looked at high resolution molecular images of the joints of people with rheumatoid arthritis in long-term remission.
Scientists learned that the membrane that protects and lubricates joints appeared normal in these patients in contrast to the inflamed, swollen joints of severe arthritis.
They also found a crucial difference in the functions of cells called macrophages between patients in disease remission compared to patients with active arthritis.
In active arthritis, these macrophages arrived from blood and caused inflammation and joint damage, while those in long-term remission exhibited a different type of macrophage that could resolve inflammation and instruct adjacent cells to repair the joint.
Lead author Dr Mariola Kurowska-Stolarska, of RACE, said: “The result of this study is a credit to the vision and teamwork of our multinational collaborators.
"We identified different types of macrophages, and our goal now is to discover treatments that will encourage development of resolving macrophages in the joint.
“This would be a useful additional strategy to current treatments that calm-down the aggressive macrophages in arthritis.
"In the meantime, the relative numbers of resolving macrophages or aggressive macrophages in the synovium, or joint, might be a good predictor of flare and an indicator of arthritis patients maintaining remission.”
Professor Iain McInnes, Director of iii and Chair of the RACE Management Committee, said: “For many years we have focussed our research efforts on the pathways that switch on inflammation in the joints of people with rheumatoid arthritis – and this new study is remarkable in showing us how natural resolution of inflammation occurs.
"This gives us new clues as to how we can best design new treatments to achieve remission - our long-standing goal!”
Natalie Carter, Head of Research Engagement at Versus Arthritis, said: “Of people experiencing chronic pain every day, eight in 10 of them have arthritis.
"Despite improved treatments for inflammatory arthritis there are still many people with the condition who live in persistent pain because they don’t respond to new therapies.
“For people with rheumatoid arthritis, tackling inflammation early and effectively is the surest way to ensure that joint damage is kept to a minimum and they can lead full and active lives.
“By finding the exact immune cells present when people with arthritis go into remission after successful treatment, we have a potential key to open up a future world where people can move swiftly from the persistent pain caused by arthritis to treatments that work best for them.”
Distinct synovial tissue macrophage subsets regulate inflammation and remission in rheumatoid arthritis
- Stefano Alivernini, Lucy MacDonald, Aziza Elmesmari, Samuel Finlay, Barbara Tolusso, Maria Rita Gigante, Luca Petricca, Clara Di Mario, Laura Bui, Simone Perniola, Moustafa Attar, Marco Gessi, Anna Laura Fedele, Sabarinadh Chilaka, Domenico Somma, Stephen N. Sansom, Andrew Filer, Charles McSharry, Neal L. Millar, Kristina Kirschner, Alessandra Nerviani, Myles J. Lewis, Costantino Pitzalis, Andrew R. Clark, Gianfranco Ferraccioli, Irina Udalova, Christopher D. Buckley, Elisa Gremese, Iain B. McInnes, Thomas D. Otto & Mariola Kurowska-Stolarska
Distinct synovial tissue macrophage subsets regulate inflammation and remission in rheumatoid arthritis. Nat Med (2020). https://doi.org/10.1038/s41591-020-0939-8
The study was funded by Versus Arthritis UK, Wellcome Trust, and Italian Ministry of Health.
Enquiries: ali.howard@glasgow.ac.uk or elizabeth.mcmeekin@glasgow.ac.uk / 0141 330 6557 or 0141 330 4831
First published: 1 July 2020

