Experience as PhD student and NHS public health professional
Published: 23 June 2020
Our PhD Student and Clinical Research Fellow Rachel Thomson reflects on being a PhD student & public health professional called on to assist with the pandemic.
Published 23rd June 2020
By Rachel Thomson.
This piece is part of a series published in IHAWKES collecting the experiences of researchers during the current COVID-19 pandemic.
is a Wellcome Trust Clinical Research Fellow who started a PhD modelling the impacts of welfare policies on population mental health at the University of Glasgow in September 2019. Her clinical background is in public health medicine, and since March 2020 she has returned to clinical practice on a part-time basis to assist with the public health response to COVID-19 in NHS Ayrshire & Arran (A&A). In the following piece, Rachel reflects on her experience of this time as PhD student and public health professional.

Since COVID-19 became woven into the fabric of our everyday lives, I’ve lost count of the number of people who’ve joked that at least now people will know what I do for a living. It’s true that of all the medical specialties public health isn’t one of the sexiest, and so it’s generally not well understood. No heroic life-saving surgeries, no stethoscopes or scrubs – instead, lots of spreadsheets, stats, and politics with a small ‘p’. Before the COVID-19 pandemic, my friends often joked during the (infrequent) times I was ‘on call’ for public health that if I actually did get paged, it must mean the end of the world as we knew it. Turns out they weren’t entirely wrong.
The realities of ‘peacetime’ public health are very different from the past six months; COVID-19 has tested the public health workforce like little before. From the relatively sheltered world of academia, I watched as my former colleagues in NHS A&A’s public health department (where I’d been training as a registrar since 2016) moved from what’s typically a fairly comfortable 9-to-5 job, to one which began to push the boundaries of work-life balance in ways I only recognised from my time working in acute hospitals.
In mid-December 2019, awareness began to spread from Wuhan, China to Scotland’s local and national public health systems of what was then only characterised as an emerging new severe viral pneumonia. As the potential for this to become a global threat became clearer over the following months, the workload within our tiny Health Protection Team increased exponentially, mushrooming out to pull in staff from other areas alarmingly quickly. Within the space of a few short weeks following news headlines in February, I moved from thinking ‘it’d have to get really bad before they’d need to draft me back in’ to ‘I can’t in good conscience not go back right now’. At that point I agreed with my PhD supervisors and my funder that I’d return to NHS service three days a week, keeping the remaining two days for my academic work. I officially started back on 20th March 2020; just three days later the UK declared a lockdown, and I found myself right in the thick of it.
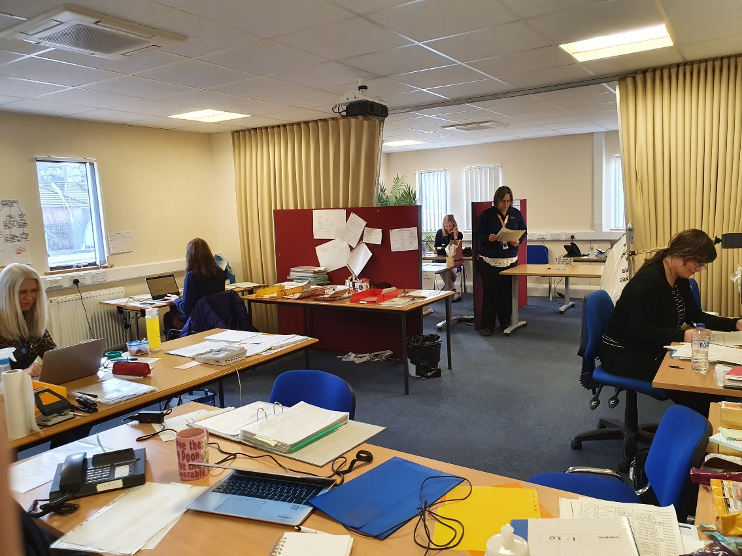
The NHS Ayrshire & Arran COVID19 Control Centre: a socially distanced workplace!
On my NHS days I’m based in the NHS A&A COVID-19 Control Centre in Ayr, working alongside an absolutely incredible team of public health nurses, practitioners, and consultants. Our role is primarily managing community-based COVID-19 outbreaks in closed settings (e.g. care homes and workplaces), though we’re often contacted about wider COVID-related concerns by worried members of the public or key workers. As of 28th May we are also the escalation point for contact tracing of complex cases in Ayrshire as part of Scotland’s new NHS Test and Protect system, managing any positive COVID-19 cases who work or live within closed settings. We’re open seven days a week, which has meant that I’ve worked six-day weeks about half of the time since I started – there are few of us to spread the work between.
I’m not sure what I was expecting, but the volume and pace of the work has been relentless. One of the difficult aspects of our role is that we’re the ones people come to for help interpreting the latest guidance on infection control, personal protective equipment (PPE), or access to testing, but we often have little or no warning of the almost daily changes. As you can imagine, that doesn’t always make for happy phone conversations. Before I realised how bad it was for my mental health, I got into the habit of religiously listening to the daily press briefings in the car on the way home from work, and consuming every piece of news I’d missed in the evenings, just so I was prepared for what the calls would inevitably be about the next day. I don’t want to get into a commentary on how the pandemic has been managed – that’s a whole other blog article, and others have already written it much better than I could. But I can at least say that too often, those of us working on the public health front line have found ourselves having to rapidly act on policy changes where we simply didn’t have access to the evidence underlying them. In a specialty that prides itself on being evidence-based at all times, that’s a very uncomfortable place to be.

Taking the time to clear our heads: Lead Health Protection Nurse Fiona and I pausing on a busy Saturday afternoon to walk through the Ayr Hospital grounds
However, the best way to try and remedy those kinds of difficulties is to have a strong, supportive team around you, and our team is truly the best. At the behest of our leads we’ve had some extremely frank discussions about how challenging we’re finding things, with a focus on how we can support each other. We take time to check in with each other when we see someone is struggling; we volunteer to hold the fort when someone just needs a minute; we force each other to stop for a cup of coffee or a breath. During the peak of the epidemic, the most frequent precursors to such interventions were our discussions with care homes – speaking daily to managers and nursing staff devastated by the loss of their residents, many of whom they’ve known for years, it’s impossible not to be personally affected. That can take a toll on your own well-being in a way that I’ve become unused to since leaving hospital medicine. If we didn’t talk openly and support each other, we wouldn’t be able to keep moving onto the next call and the one after that, and keeping moving is essential. As we often remind each other, for those of us in public health this isn’t going to be a sprint – it’s a marathon, and we’ll have to persevere until we either contact trace the virus out of existence or find a vaccine.

Obligatory photo of my ‘working from home’ set-up, with bonus cat tax
My PhD hasn’t disappeared in all of this though: far from it! If anything, my topic – predicting the impacts of changes to welfare policies on mental health – has become increasingly relevant in a post-COVID world. During my academic days I’m continuing my work on a systematic review summarising literature on how changes in income affect mental health, and trying not to lose momentum despite having to juggle this with my clinical work, which often bleeds into evenings and weekends. As my lead PhD supervisor is from a clinical public health background too, I’ve also been fortunate enough to be able to contribute to some additional COVID-related research led by Public Health Scotland, studying how the economic mitigation measures such as changes to Universal Credit and the furlough scheme may impact on population health. It’s been hard to fit everything in, but it’s also really valuable to have something else to focus on, reminding me that the world beyond the Control Centre still exists.
I’m aware that my lockdown experience so far has been pretty atypical, both for a PGR student and for a clinician, and though I’ve focused a lot on the challenges here there are still many ways in which I think I’ve lucked out. I’ve been able to leave my home to travel to work in person, which means I’ve had regular face-to-face contact that so many of my friends and family have been denied for months. My PhD project is primarily secondary data analysis, so I’m not having to completely overhaul my plans like those who can’t collect their data due to lockdown. I’ve been able to reduce my academic commitment with the full support of my funder and I’m still early in my PhD, so I don’t have the acute worries about extensions I know other PGRs are facing right now. And, unlike my friends in other medical specialties, I’m protected from the worries and stress that go along with providing direct patient care during a pandemic, including the heightened fears of becoming infected yourself.
While admittedly it has been a difficult few months in many ways, it has been incredible to see first-hand how those working in health and social care have rallied in response to the pandemic. It’s impossible to predict what will come next, after this odd ‘eye of the storm’ moment with case numbers falling, temperatures rising, and adherence to lockdown waning, but I know that despite our collective exhaustion we will face it with equal determination. I’m acutely aware that this is probably – hopefully – the most significant public health emergency I will contribute to in my working life. At this stage, I can honestly say I’m grateful to have had the opportunity to dust off my figurative stethoscope and lend a hand.
The views expressed in this article are those of the author and do not necessarily reflect those of NHS Ayrshire & Arran or the University of Glasgow.
First published: 23 June 2020
<< 2020

