Glasgow team will transform bowel cancer screening into a precision medicine tool using AI
Published: 3 July 2020
The University of Glasgow, in collaboration with the NHS and Scottish tech companies, will lead a £3.37m project to transform bowel cancer screening in the UK by developing a precision diagnostic tool that uses artificial intelligence to predict which patients will develop future polyps and tumours.
The University of Glasgow, in collaboration with the NHS and Scottish tech companies, will lead a £3.37m project to transform bowel cancer screening in the UK by developing a precision diagnostic tool that uses artificial intelligence to predict which patients will develop future polyps and tumours.
The INCISE* project – made possible with £2.3m of government funding provided through UK Research and Innovation’s (UKRI) industrial strategy challenge fund and a further £1.1m from University of Glasgow and industry partners – will improve cancer detection while reducing the number of people needing repeated colonoscopy – a procedure patients find unpleasant, which also carries a risk of complications. It will also improve access to colonoscopy for others and reduce costs to the NHS.
The UKRI funding is part of £16 million of new funding announced today by Science Minister Amanda Solloway
Bowel cancer screening is used to find tumours and pre-cancerous lesions, or polyps, in patients without symptoms. The aim of screening is both to identify cancers early – making them easier to treat successfully – and if possible to remove them while they are still polyps.
In Scotland, adults at an appropriate age are invited to submit a stool sample by post, and if traces of blood are detected, they are invited to have a colonoscopy, which is a more detailed test. At colonoscopy, around one in 20 people are found to have cancer, while one in three have polyps. Around half of these patients will go on to develop new polyps, so all are currently scheduled for a future colonoscopy.
Current guidelines help clinicians decide when each patient needs a further colonoscopy. However, these guidelines are not accurate, meaning that many people undergo unnecessary and invasive procedures. The new precision tool will identify patients who would benefit the most from colonoscopy, so they are seen earlier and any cancer can be treated sooner.
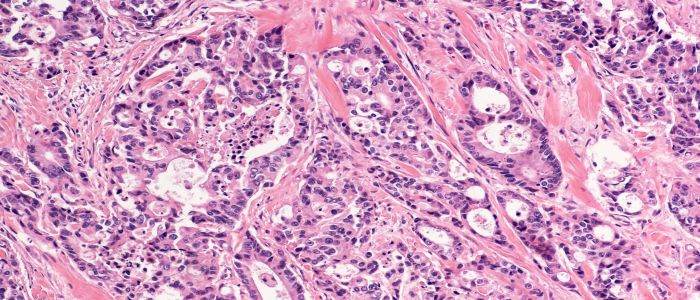
INCISE will combine polyp tissue and data from the NHS Greater Glasgow & Clyde Scottish Bowel Cancer Screening Programme to train algorithms that predict patients’ future risk. Researchers will combine information about specific changes in the polyp’s structure, seen under the microscope and analysed using deep learning, with new analysis of the genetic mutations that cause polyps to grow.
Professor Joanne Edwards, Professor of Translational Cancer Pathology at the University’s Institute of Cancer Sciences, said: “We are thrilled to receive this support and funding from Innovate UK, which will help us develop a programme that will hugely benefit both patients and our NHS.
“UofG has wide experience in all aspects of colon cancer. By combining our knowledge with industry partners and the NHS, we can harness the power of artificial intelligence to assess which patients are prone to polyps and need further colonoscopies.
“By better predicting the needs of individuals, we can help patients avoid procedures that do not benefit them, while reducing the burden and cost to the NHS.”
Industry partners for the programme include Canon Medical Research Europe, OracleBio (who will develop the deep learning digital pathology methodology) and BioClavis (who will identify the gene signatures that predict polyp behaviour).
The team from Canon Medical will integrate the results of the programme into their ‘clinical cockpit’ – a digital suite that integrates patient data to help physicians and other clinical specialists. This is also being developed for other diseases as part of iCAIRD*, Scotland’s £15.8m UofG-led artificial intelligence health research centre, which involves partners from across academia, the NHS and industry.
The funding, delivered through the Industrial Strategy Challenge Fund, is part of a government programme in data to early diagnosis and precision medicine. Led by the Medical Research Council (MRC) and UK Research and Innovation’s (UKRI) Innovate UK, it forms part of the government’s commitment to increase research and development investment to 2.4% of GDP by 2027.
UK Government Minister for Scotland Iain Stewart said: “It’s great that the UK Government and Cancer Research UK have joined forces to provide £16 million funding to speed up life-saving cancer diagnoses across the UK.
“Here in Scotland this will help fund a cutting-edge project led by the University of Glasgow on bowel cancer, which sadly remains the second largest cause of cancer related deaths.
“This all-important funding will allow our world class academic and research teams in Glasgow to develop the specialist technology needed to detect this life threatening disease not only earlier but with more accuracy. This will make a real difference to individuals and their families and help save lives not just in Scotland but the wider UK.”
UKRI is partnering with Cancer Research UK, which is making a £3m contribution to the cancer-focused projects.
*INCISE stands for INtegrated TeChnologies for Improved Polyp SurveillancE.
*iCAIRD stands for Industrial Centre for Artificial Intelligence Research in Digital Diagnostics.
Enquiries: ali.howard@glasgow.ac.uk or elizabeth.mcmeekin@glasgow.ac.uk / 0141 330 6557 or 0141 330 4831
First published: 3 July 2020
<< July

